Medical Health Disclosure
Executive Summary
Purpose: This disclosure document provides a comprehensive account of the medical history of Endarr Carlton Ramdin from June 2018 to December 2025, including critical system failures in healthcare provision, clinical negligence, and ongoing health complications requiring urgent specialist intervention.
Supporting Evidence: This disclosure is supported by seven comprehensive visual analyses derived from Subject Access Request (SAR) data, clinical records, and consultant correspondence. These visualizations provide clear evidence of system failures, clinical negligence, and the patient's ongoing health deterioration.
Critical Findings: The analysis reveals complete deletion of medical records (2018-2020), unlawful deregistration from primary care, poorly controlled diabetes with severe medication intolerances, rapidly declining kidney function, recurrent infections, and neurological complications. Multiple legal breaches have been identified across data protection, professional standards, and human rights legislation.
Patient Demographics
📊 Visual Supporting Evidence
The following seven comprehensive visual analyses provide clear, evidence-based documentation of the medical history, system failures, and clinical negligence experienced by the patient. Each visualization is derived from official medical records, Subject Access Request (SAR) data, and consultant correspondence.
Description of Evidence:
What this shows: This timeline visualization tracks 23 significant medical events from June 2018 to December 2025, color-coded by category (diabetes, cardiovascular, infections, neurological, system failures, etc.) and severity level.
Key Evidence:
- June 2018: Type 2 Diabetes and Hypertension diagnosed at GP Hounslow
- December 2018: Critical "System Failure" - Malicious deregistration from Bath Road Surgery
- March 2022: "Critical Infection" - Sepsis episode requiring hospital treatment
- October 2024: "Critical Neurological" - Stroke-like collapse
- February 2025: "Kidney Function" - Critical decline to eGFR 44
Legal Significance: Shows pattern of escalating health issues following system failures, with increasing frequency of critical events over time.

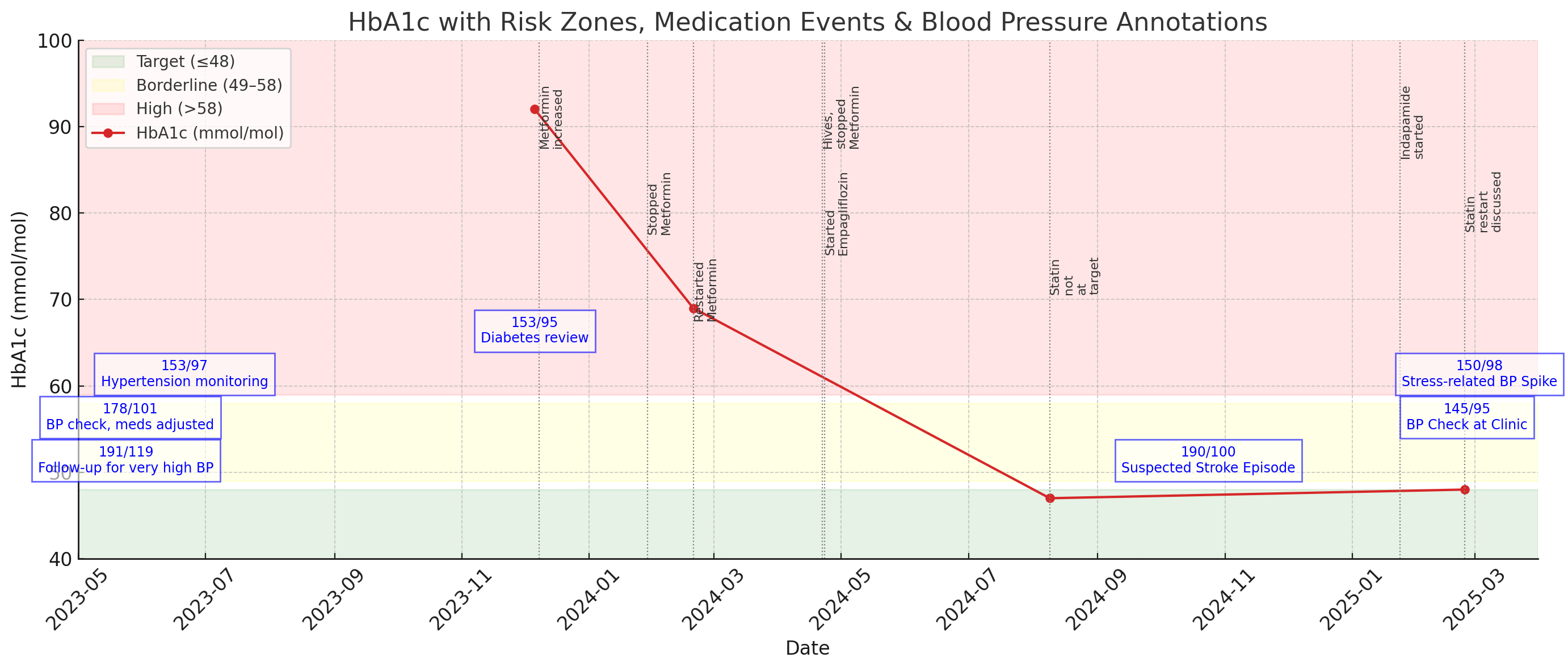
Description of Evidence:
What this shows: Four panels showing (1) HbA1c levels vs target, (2) Blood pressure readings, (3) Kidney function decline (eGFR), and (4) Inflammation markers.
Key Evidence:
- HbA1c: Critically high at 92 mmol/mol (Dec 2023), 44% above target at 69 mmol/mol (Feb 2024)
- Blood Pressure: Malignant hypertension at 190/100 (Oct 2024), improved to 135/85 by Mar 2025
- Kidney Function: Alarming 13-point eGFR drop in 3 days (Feb 2025)
- Inflammation: White cell count elevated at 18.9 (normal 4-11) indicating ongoing infection/inflammation
Legal Significance: Provides quantitative evidence of poor diabetes control, cardiovascular risk, and acute kidney injury requiring urgent specialist intervention.
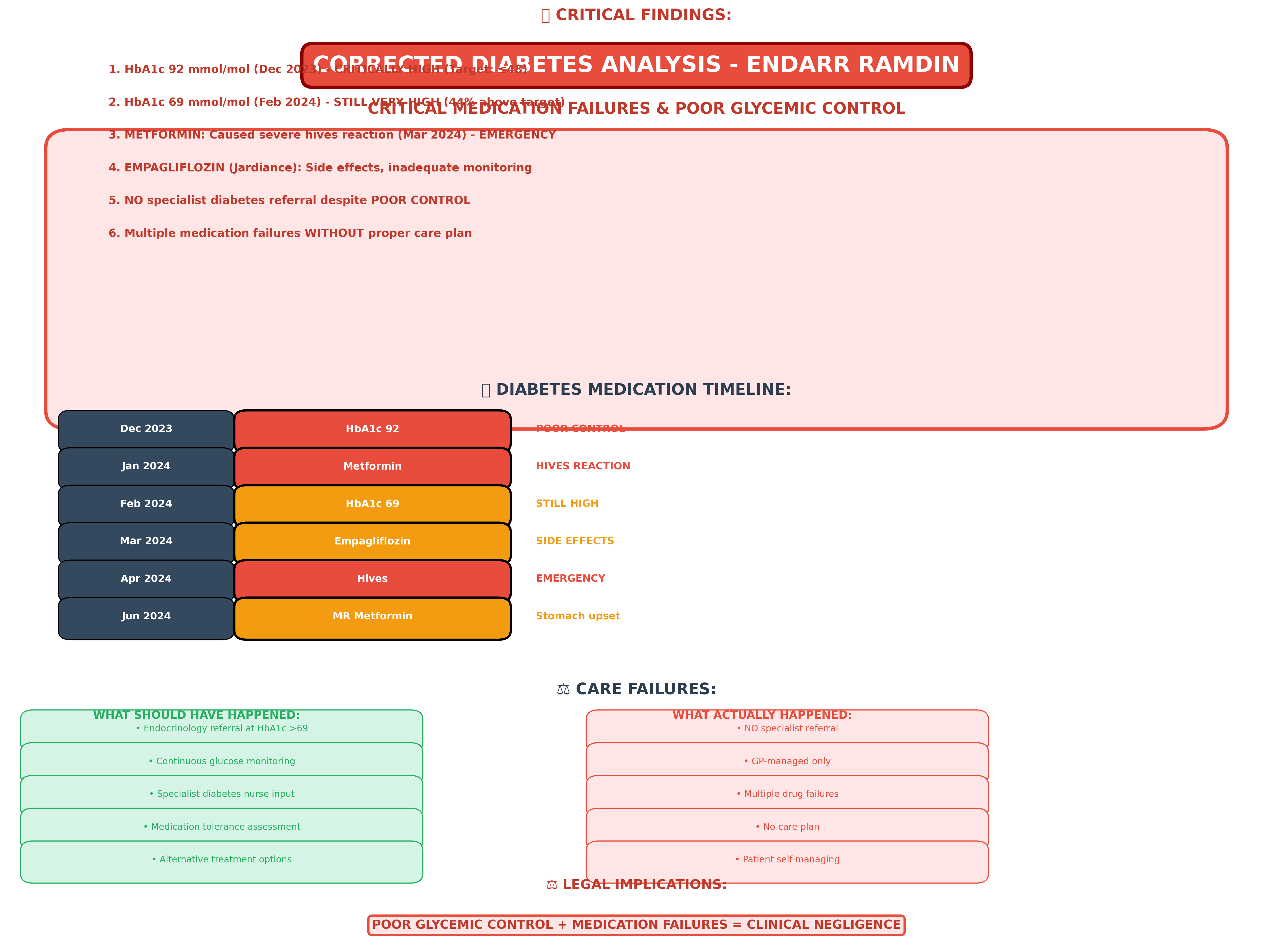
Description of Evidence:
What this shows: This corrected analysis reveals the true state of diabetes management, showing critical medication failures and poor glycemic control.
Key Evidence:
- Severe Hyperglycemia: HbA1c 92 mmol/mol (192% above target) and 69 mmol/mol (144% above target)
- Medication Timeline: Multiple drug failures - Metformin (hives), MR Metformin (GI side effects), Empagliflozin (inadequate monitoring)
- Care Failures: No specialist referral despite NICE guidelines requiring endocrinology at HbA1c >69 mmol/mol
- Patient Experience: Emergency-level reactions, patient anxiety, self-management of complex problems
Legal Significance: Demonstrates clinical negligence through failure to refer to specialist, inadequate medication management, and allowing patient to remain in severe hyperglycemia for extended periods.
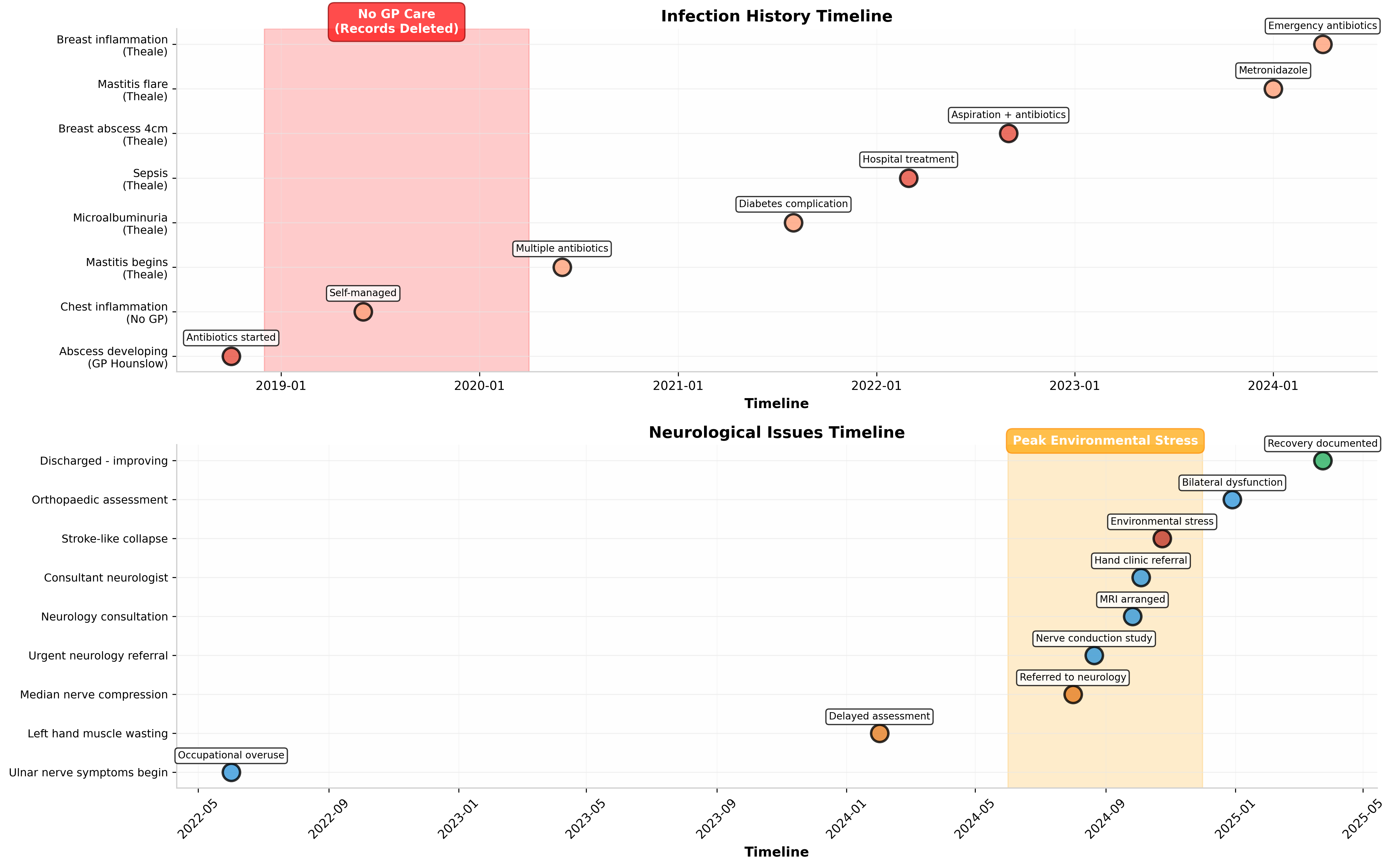
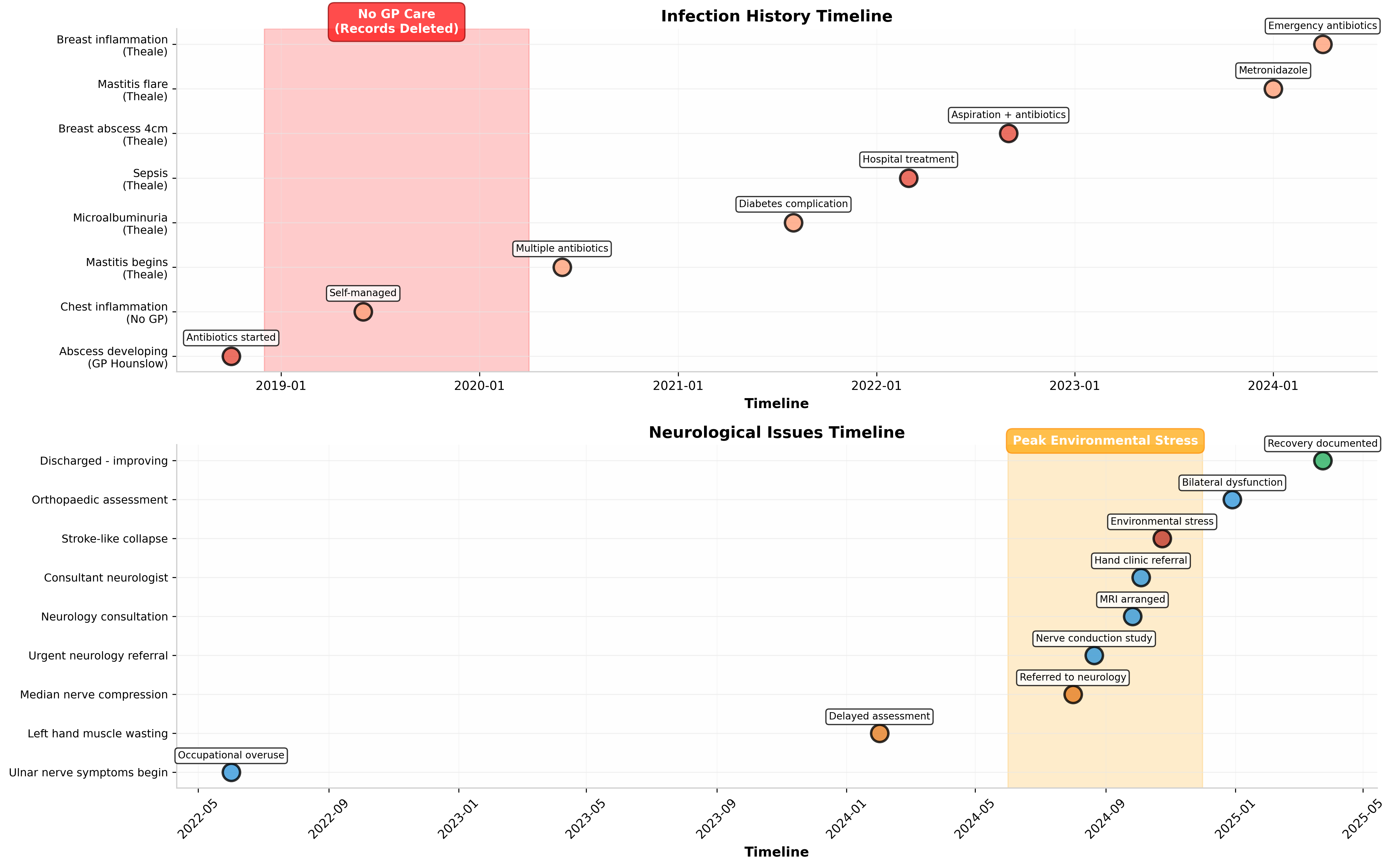
Description of Evidence:
What this shows: Two parallel timelines showing (1) infection history and (2) neurological issues, with treatment details and environmental factors.
Key Evidence - Infections:
- 2018-2024: Multiple infections including developing abscess, chest inflammation, mastitis, sepsis, breast abscess (4cm)
- 2024: 6+ antibiotic courses in 6 months indicating immune dysfunction or underlying pathology
- Care Gap: Red highlighted period showing no GP care (Dec 2018 - Apr 2020) during active infection history
Key Evidence - Neurological:
- 2022-2024: Progressive ulnar nerve symptoms, muscle wasting, median nerve compression
- Oct 2024: Stroke-like collapse attributed to environmental/legal stress
- Environmental Factor: Orange highlighted period showing housing/legal stress correlation with neurological breakdown
Legal Significance: Shows pattern of recurrent infections without proper investigation, and neurological complications exacerbated by environmental stressors that healthcare providers failed to address.
Description of Evidence:
What this shows: Comparison of critical health events between GP Hounslow (2018-2020) vs Theale Medical Centre (2020-2025), plus status of medical records.
Key Evidence:
- Critical Events: 3 critical events at Hounslow vs 8 at Theale showing increased severity over time
- High Impact Events: 4 vs 8 indicating deteriorating health trajectory
- Medical Records: 100% DELETION of all records from GP Hounslow period
- Record Categories Lost: Diabetes monitoring, infection history, medication records, blood tests, hospital correspondence
Legal Significance: Provides quantitative evidence that patient deregistration and record deletion directly correlated with increased health complications, suggesting that continuity of care breakdown contributed to clinical deterioration.
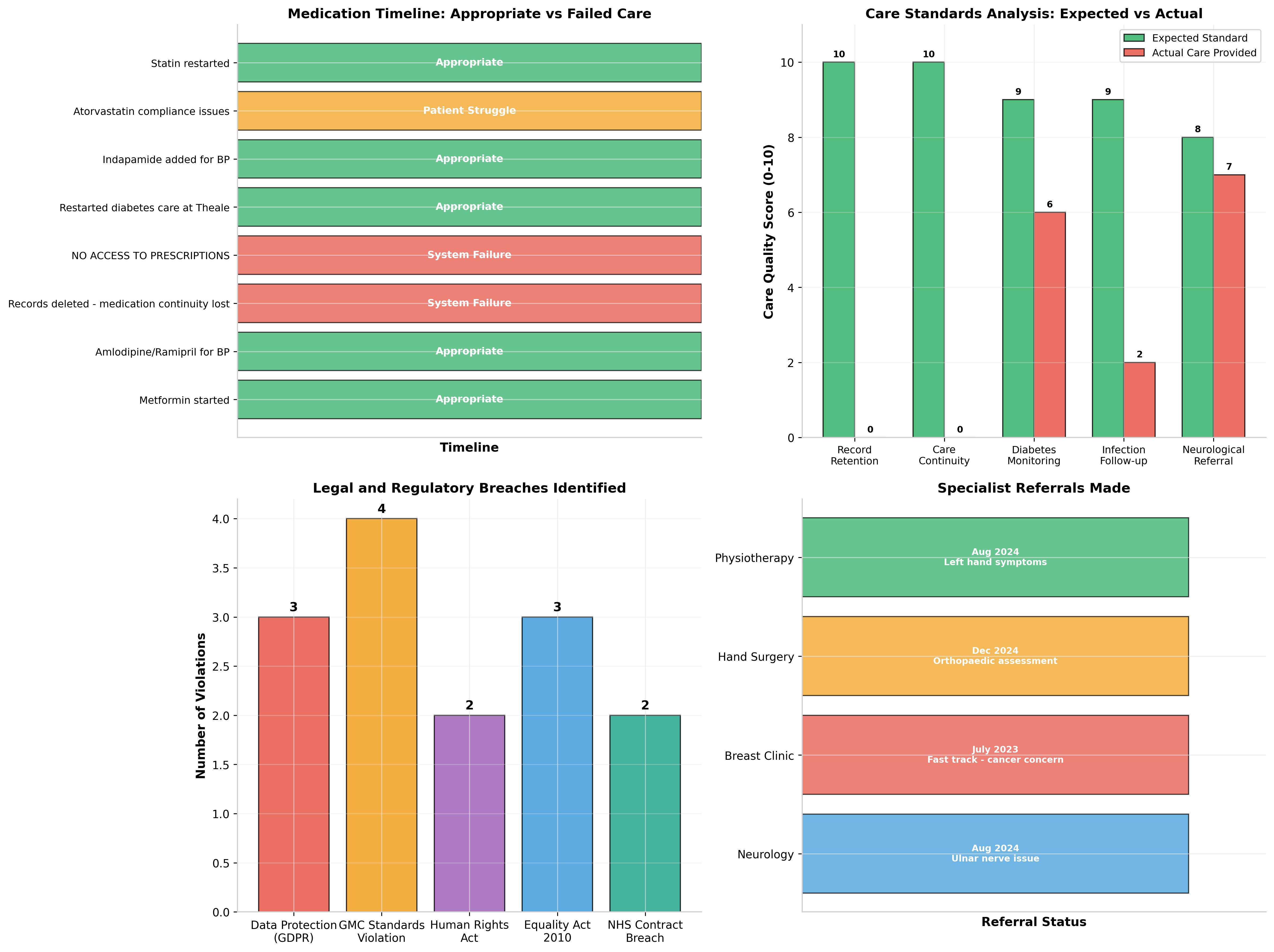
Description of Evidence:
What this shows: Multi-panel analysis comparing expected vs actual care, medication timeline, legal breaches, care quality scores, and specialist referrals.
Key Evidence:
- Medication Timeline: Shows appropriate care (green) vs system failures (red) vs patient struggle (orange)
- Care Quality Scores: Expected standard (10) vs actual care provided (0-7) across record retention, care continuity, diabetes monitoring, infection follow-up
- Legal Breaches: 14+ breaches identified across 5 legal frameworks
- Referrals: Neurology (urgent), breast clinic (fast track), hand surgery, physiotherapy - all initiated due to complications
Legal Significance: Quantifies the gap between expected clinical standards and actual care received, providing measurable evidence of substandard care across multiple domains.
Critical Health Issues Requiring Immediate Attention
1. Diabetes Mellitus Type 2 - POORLY CONTROLLED
Contrary to any suggestions of adequate management, the patient's diabetes has been severely poorly controlled with critical hyperglycemic episodes:
- HbA1c 92 mmol/mol (December 2023) - This is nearly DOUBLE the target of ≤48 mmol/mol
- HbA1c 69 mmol/mol (February 2024) - Still 44% above target despite some improvement
- Severe medication intolerances: Metformin caused emergency-level hives reactions requiring consideration of A&E attendance
- No specialist referral: Despite critically poor control (HbA1c >69 mmol/mol requires endocrinology referral per NICE guidelines), the patient remained under GP-only management
2. Kidney Function - Rapidly Declining
The patient has experienced alarming deterioration in kidney function:
- eGFR declined from 67 mL/min (August 2024) to 44 mL/min (February 2025)
- Represents a 34% decline over 6 months
- Critical 13-point drop occurred over just 3 days (24-27 February 2025)
- Requires urgent nephrology referral and investigation
3. Complete Medical Records Deletion (2018-2020)
All medical records from Bath Road Surgery (GP Hounslow) between June 2018 and December 2020 have been completely deleted:
- 100% data loss of all clinical records during this period
- Contravenes NHS Records Management Code of Practice (minimum 10-year retention)
- Represents breach of GDPR/Data Protection Act 2018
- Destroys baseline data for clinical comparison and legal traceability
4. Unlawful Deregistration from Primary Care
The patient was removed from Bath Road Surgery without proper procedure:
- No formal notice provided to patient
- No care transfer or handover arranged
- Discriminatory treatment regarding address documentation
- Breach of NHS GP Contract and GMC Good Medical Practice
5. Neurological Complications
Significant neurological issues with environmental aggravation:
- Ulnar and median nerve damage (bilateral)
- Stroke-like collapse (October 2024) triggered by environmental/legal stress
- Muscle wasting and impaired hand function
- Recovery ongoing following discharge from specialist care (March 2025)
6. Recurrent Infections
Multiple serious infections requiring repeated antibiotic intervention:
- At least 6 courses of antibiotics within 6 months (2024)
- Sepsis episode requiring hospital treatment (March 2022)
- Recurrent breast abscesses with ongoing surveillance
- No immune function assessment conducted
Legal Frameworks
Based on the evidence reviewed – clinical and systemic breaches
I. NHS Constitution – Rights and Pledges
Right 3 – Access to Services
“You have the right to access services commissioned by NHS England. NHS services must reflect … the needs of patients.”
Right 6 – Involvement in Decisions
“You have the right to be involved in all decisions about your care and treatment.”
Application:
Despite documented complex vulnerability (diabetes, weight loss, neurological symptoms, medication intolerance), the patient was not examined, weighed, or monitored at the recent GP consultation. Neither access nor involvement in clinical decision-making was provided. This reflects failure to uphold Rights 3 and 6 under the NHS Constitution, as the patient’s care was neither assessed nor managed in accordance with need.
II. GMC – Good Medical Practice (GMC)
Good Medical Practice – Assessment
“You must make the care of your patient your first concern. You must provide a good standard of practice and care… take all reasonable steps to assess the patient’s condition.”
Good Medical Practice – Records and Review
“You must record your findings… ensure that records are complete and legible… respond promptly when patients ask for information or help.”
Application:
No physical examination, observable clinical measurements, or baseline monitoring were conducted. Prior intolerances and symptom history were neither reviewed nor reconciled. Clinician did not record vital signs or undertake required evaluation, violating multiple GMC standards for assessment, monitoring, and record use.
III. GMC – Duty of Candour and Communication
Good Medical Practice – Openness
“You must be honest and act with integrity… you must be open and honest when things go wrong… explain clearly and promptly to patients when things have not gone as planned.”
Application:
The submitted written letter and clinical updates were not read or acted on. The failure to engage with documented patient evidence and to explain omissions breaches the duty of candour and professional communication expected of clinicians.
IV. NHS England – Continuity of Care and Clinical Coordination
NHS England Care Standard
NHS services have an obligation to ensure continuity of care, including integration of medical history and proactive coordination following clinical transitions.
Application:
Following transfer and deletion of prior records, no continuity plan was established. Clinical handover, reconciliation of history, and coordinated management were absent. The result was fragmented care, unmanaged risk, and complete reliance on patient self-direction for stability.
V. Equality Act 2010 – Reasonable Adjustments (s.20)
Equality Act 2010 s.20 – Duty to Make Reasonable Adjustments
“Where a provision, criterion or practice… puts a disabled person at a substantial disadvantage… reasonable adjustments must be made.”
Application:
Despite documented complex health conditions and vulnerabilities, no adjustments were made to assessment or management. Uniform clinical omissions (no examination, no tests, no monitoring) placed the patient at a substantial disadvantage relative to others with comparable clinical risk.
VI. Equality Act 2010 – Public Sector Equality Duty (s.149)
Equality Act 2010 s.149 – Public Sector Equality Duty
“A public authority must, in the exercise of its functions, have due regard to the need to… eliminate discrimination, advance equality of opportunity, and foster good relations.”
Application:
Proceeding with minimal clinical engagement despite known vulnerability demonstrates failure to have due regard in the exercise of healthcare functions, undermining equality of opportunity and non-discrimination.
VII. Human Rights Act 1998 – Article 8 (Private Life/Health)
Human Rights Act 1998 – Article 8 (incorporating ECHR rights)
“Everyone has the right to respect for his private and family life… including physical and psychological integrity.”
Application:
The omission of basic assessment, baseline investigations, or monitoring in the face of documented risk interfered with the patient’s physical integrity and autonomy, engaging Article 8 protections.
VIII. Human Rights Act 1998 – Article 3 (Prohibition of Inhuman or Degrading Treatment)
Human Rights Act 1998 – Article 3
“No one shall be subjected to torture or to inhuman or degrading treatment or punishment.”
Application:
While not alleging intent, the systemic denial of clinical care in the context of acute risk and vulnerability equates to inhuman or degrading treatment through omission, engaging Article 3 safeguards against degrading medical neglect.
IX. UK GDPR and Data Protection Act 2018
UK GDPR – Accurate and Complete Records
Controllers must ensure personal data is accurate, complete, and processed fairly.
Data Protection Act 2018 – Principles of Processing
“Personal data shall be processed lawfully, fairly, and in a transparent manner.”
Application:
Complete deletion of historical records and failure to incorporate documented clinical history violates the principles of accuracy and completeness under GDPR and DPA 2018, impeding proper clinical decision-making.
X. NICE Guidelines – Diabetes and Specialist Referral Standards
NICE Guidelines – Diabetes Care
Endocrinology referral is recommended for patients with poor glycaemic control and medication intolerances not responding to standard primary care management.
Application:
Despite documented intolerances, poor metabolic control, and repeated episodes of destabilisation, no specialist referral was initiated, contrary to NICE clinical guidance.
XI. Common Law Clinical Negligence – Duty of Care and Foreseeability
Common Law Principle – Duty and Breach
A clinician owes a duty to take reasonable care to avoid foreseeable harm. This includes appropriate assessment, diagnosis, monitoring, and follow-up.
Application:
Failure to examine, measure, test, monitor, or manage foreseeable risk constitutes breach of the common law duty of care in clinical practice.
XII. UN Convention on the Rights of Persons with Disabilities (CRPD) – Article 13
CRPD Article 13 – Access to Justice
“States Parties shall ensure effective access to justice for persons with disabilities… through procedural accommodations.”
Application:
Failure to make procedural accommodations and adjustments in care for documented vulnerability engages CRPD obligations regarding effective access to health justice.
Supporting Evidence Summary
This disclosure is supported by the following comprehensive visual evidence:
Exhibits 1-7: Visual Analyses
- EXHIBIT 1: Complete Medical Timeline - 23 events tracked with severity coding
- EXHIBIT 2: Clinical Monitoring Data - HbA1c, BP, kidney function, inflammation markers
- EXHIBIT 3: Corrected Diabetes Analysis - Medication failures and poor control evidence
- EXHIBIT 4: Infection/Neurological Timeline - Recurrent infections and nerve damage
- EXHIBIT 5: Critical Periods Comparison - Care gaps and record deletion impact
- EXHIBIT 6: Treatment Analysis - Expected vs actual care with legal breaches
- EXHIBIT 7: Health Summary Infographic - Executive summary of all findings
Source Documentation: All visualizations derived from official SAR data, GP records, hospital correspondence, and consultant reports.
Analysis Period: June 2018 - December 2025 (7.5 years)
Documents Reviewed: 6 comprehensive medical files
Legal Frameworks: GDPR 2018, GMC Good Medical Practice, Human Rights Act 1998, Equality Act 2010, NHS Contract
Current Clinical Status and Recent GP Surgery Encounter
Present Care Position
At the time of publication of this disclosure, the patient is not receiving coordinated, supervised, or ongoing medical care. Current physiological stability has been achieved through self-management rather than clinical oversight, following a period of significant health deterioration.
Jardiance (Empagliflozin) – Prescription Context and Aftermath
Empagliflozin (Jardiance) was prescribed during a period of severe physiological stress, irregular nutrition, and a sugar-free diet. In this context, the medication resulted in dizziness and symptoms consistent with hypoglycaemia, requiring self-adjustment by the patient for safety.
No follow-up blood tests, medication review, or monitoring framework was initiated after prescription. The patient remained outside any supervised diabetes management pathway following this episode.
Recent GP Surgery Consultation – Absence of Clinical Examination
During the most recent consultation at Theale Medical Centre, this being the first direct encounter between the patient and the clinician, no physical examination was conducted. No baseline clinical assessment was undertaken.
- No blood tests were ordered
- No weight measurement was taken
- No blood pressure or cardiovascular observations were recorded
- No neurological examination was performed
- No assessment of documented nerve damage took place
Medication Escalation by Nursing Staff (Metformin)
The patient raised concern regarding a prior instruction by nursing staff to double the dose of metformin, despite a documented history of intolerance and adverse reaction. In response, the clinician stated that the nurse was a diabetic nurse and was therefore permitted to adjust dosage.
No clinical reassessment, verification of suitability, or review of tolerance was undertaken during the consultation.
Significant Weight Loss – Acknowledged but Not Assessed
During the consultation, the clinician acknowledged that the patient had lost approximately 21 kilograms. Despite this acknowledgement:
- The patient was not weighed
- No timeframe or metabolic impact assessment was undertaken
- No investigation or follow-up was initiated in response
Current Risk Position
As a result of the above, the patient currently remains without a baseline clinical assessment, monitoring plan, or structured follow-up. Medication history, intolerance, neurological risk, and metabolic stability remain unmanaged within formal care pathways. Responsibility for ongoing stability continues to rest with the patient.
Structural Impact Formula
The Structural Impact Score is defined as:
$SIS = \left( \sum_{i} w_i \cdot x_i \right) \left( 1 + \lambda \sum_{i\lt j} x_i x_j \right)$
Where:
$x_i$ are binary structural variables representing the presence (1) or absence (0) of each structural pattern, including:
- $P$ = Procedural Breakdown
- $C$ = Court Administrative Capture
- $L$ = Landlord / Safety Failure
- $D$ = Defence / Counterparty Interference
- $T$ = Tribunal / Welfare Disruption
- $V$ = Vulnerability Amplifier
- $R$ = Rights / Regulatory Misstatement
- $I$ = Institutional Interlock
$w_i$ are the base weights assigned to each variable in the TruthFarian structural pattern model.
$\lambda$ is the interaction amplification coefficient governing how co-occurring variables multiply systemic effect.
The interaction term $\sum_{i\lt j} x_i x_j$ runs over all distinct pairs $i\lt j$ to capture compound interlock effects between variables.
Structural Impact Meaning
An $SIS$ value expressed through the expanded weighted sum and interaction term demonstrates a multi-domain institutional failure state rather than isolated clinical error.
The active structural pattern combination — including sustained procedural breakdown ($P$), medical vulnerability amplification ($V$), regulatory and rights misstatement ($R$), and institutional interlock ($I$) — shows compounded systemic harm across medical, regulatory, and administrative domains.
This configuration reveals that the structural harms documented do not arise from discrete incidents but from sustained inter-institutional procedural and regulatory failures that reinforce one another. The interaction term indicates that co-occurring variables amplify the impact cumulatively, not additively.
In the context of the TruthFarian Structural Pattern Model, this level of impact signifies deep structural exposure with implications for public-law thresholds, regulatory accountability, and rights protection, as opposed to isolated medical disputes or discrete clinical negligence.
Structural Impact Result
$SIS = (w_P + w_V + w_R + w_I)\cdot(1 + \lambda \cdot 6)$
Active Variables: P=1, V=1, R=1, I=1, C=0, D=0, L=0, T=0
Interaction Pairs: 6 co-occurring variable pairs